Fungal Infection
Fungal infections, also known as mycoses, are common ailments caused by fungi that invade various parts of the body. Fungi are microscopic organisms found in the environment, such as soil, plants, and even the human body. While most fungi are harmless, some can cause infections when they overgrow and penetrate the skin, nails, hair, or mucous membranes. Fungal infections can range from mild, superficial conditions to severe, systemic illnesses. Understanding the different types, causes, and treatments of fungal infections is essential for effective management and prevention.
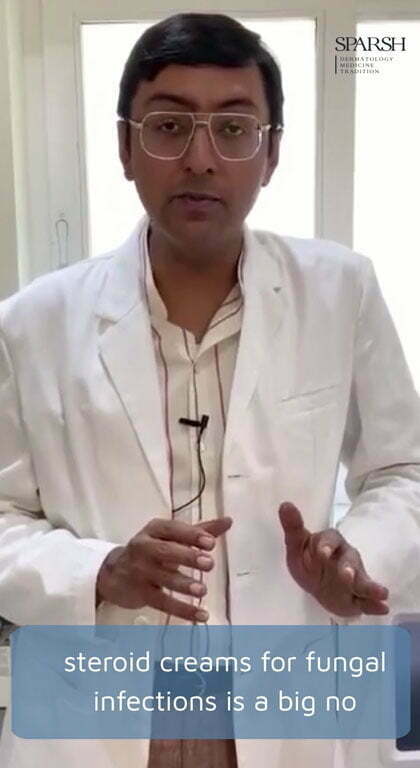
At SPARSH, we understand the concerns and discomfort associated with fungal infections. That’s why we offer a comprehensive range of treatments for all types of fungal infections. Whether you’re dealing with athlete’s foot, ringworm, jock itch, nail fungal infections, or any other fungal condition, we are here to help. Our experienced healthcare professionals are well-versed in diagnosing and treating fungal infections effectively. Don’t let the symptoms hold you back. Be confident in seeking the right treatment. Book an appointment with us today and take the first step towards restoring your skin’s health and your peace of mind.
Types of Fungal Infections
There are several types of fungal infections, each affecting different areas of the body. The most common types include:
Athlete’s Foot (Tinea Pedis): This infection affects the skin between the toes and the soles of the feet, leading to itching, burning, and scaling. It is commonly acquired in public areas like swimming pools and locker rooms.
Ringworm (Tinea Corporis): Contrary to its name, ringworm is not caused by worms but by a fungus. It appears as a circular, red rash with a raised border and can occur on the body, scalp, or groin. Direct skin-to-skin contact with an infected person or contaminated objects can lead to its transmission.
Yeast Infections: Candida is a type of yeast that naturally resides in the body, particularly in warm and moist areas like the mouth, genital area, and intestines. However, overgrowth of Candida can cause infections such as oral thrush (mouth) or vaginal yeast infections (genital area).
Jock Itch (Tinea Cruris): Jock itch affects the groin area and inner thighs, causing a red, itchy rash. It is commonly seen in athletes, people who sweat excessively, or those with compromised immune systems.
Nail Fungus (Onychomycosis): Nail fungal infections can affect the toenails or fingernails, causing them to become thick, discolored, and brittle. These infections are often challenging to treat and may require long-term management.





Causes of Fungal Infections
Fungal infections are caused by various fungi, including dermatophytes, yeasts, and molds. The following factors can contribute to the development of fungal infections:
Warm and Moist Environments: Fungi thrive in warm and moist conditions, such as sweaty shoes, damp socks, or areas with poor ventilation. These environments create an ideal breeding ground for fungal overgrowth.
Weakened Immune System: Individuals with weakened immune systems, such as those with HIV/AIDS, diabetes, or undergoing chemotherapy, are more susceptible to fungal infections. The immune system helps in fighting off fungal invaders, so a compromised immune system can’t mount an effective defense.
Direct Contact: Fungal infections are contagious and can spread through direct contact with an infected person or by touching contaminated surfaces, such as shared towels, clothes, or bedding.
Poor Hygiene: Insufficient personal hygiene practices, such as not washing hands regularly or wearing dirty clothes, can increase the risk of fungal infections.
Certain Medications: Prolonged use of antibiotics or corticosteroids can disrupt the natural balance of microorganisms in the body, leading to fungal overgrowth.
Treatments for Fungal Infections
The treatment of fungal infections depends on the type, severity, and location of the infection. Common treatment options include:
Topical Antifungal Medications: Creams, lotions, or powders containing antifungal agents can be applied directly to the affected area to kill the fungi and relieve symptoms. These are typically used for mild to moderate infections.
Oral Antifungal Medications: For more severe or widespread infections, oral antifungal medications may be prescribed. These medications work from within the body to eradicate the fungi. Treatment duration can vary from a few weeks to several months, depending on the infection.
Antifungal Nail Lacquer: In the case of nail fungal infections, antifungal nail lacquers can be applied directly to the affected nails to promote healing and prevent further spread.
Preventive Measures: To prevent fungal infections, it is important to maintain good hygiene practices, keep the skin clean and dry, avoid sharing personal items, wear breathable footwear, and use antifungal powders in susceptible areas.
Lifestyle Changes: Making certain lifestyle changes can also help in preventing fungal infections. These include wearing loose-fitting clothes, using mild soaps and detergents, and consuming a balanced diet that supports a healthy immune system.